Reproductive Health 101: Female Fertility

The World Health Organization (WHO) defines reproductive health as a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity, in all matters relating to the reproductive system and to its functions and processes.
Reproductive health implies that people are able to have a satisfying and safe sex life and that they have the capability to reproduce and the freedom to decide if, when and how often to do so.
Fertility, the capability to reproduce, is thus an integral part of reproductive health that contributes to a state of complete physical, mental and social wellbeing.
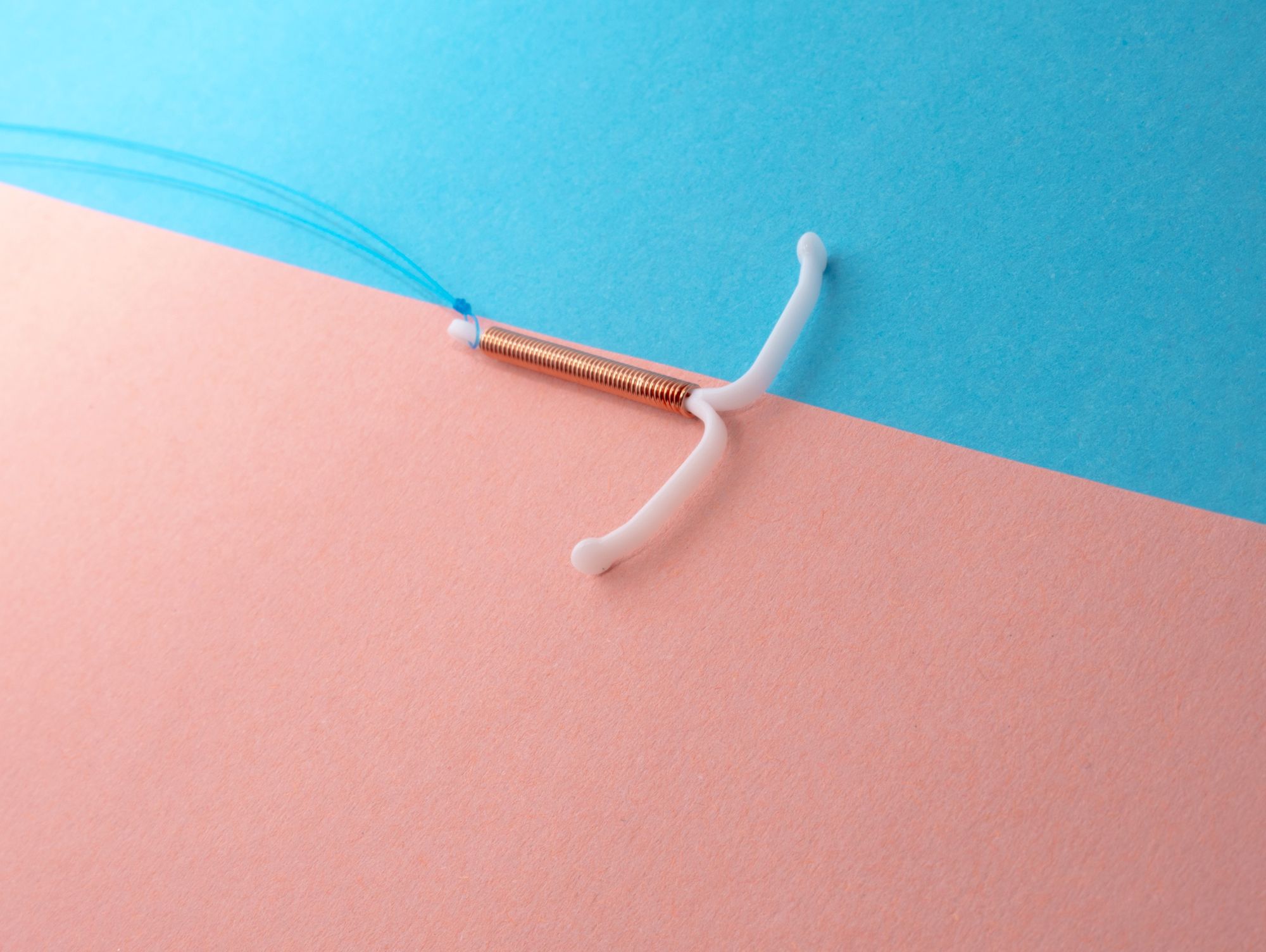
Fertility
Fertility is the ability to conceive and have children. It includes both the biological capacity to reproduce and the actual occurrence of pregnancy and childbirth. For women, fertility is the ability to get pregnant and carry a pregnancy to term, while for men, it’s the ability to produce healthy sperm that can fertilise an egg.
Fertility involves the production of viable eggs in women and sperm in men, the process of fertilisation, and the successful implantation and development of a fertilized egg in the uterus.
Infertility
Infertility is when a couple cannot conceive despite having regular unprotected intercourse for at least one year, while subfertility refers to when a couple experiences difficulty getting pregnant due to a reduced capacity to conceive, though are still able to conceive naturally.
The fertilisation process

For pregnancy to occur, every step of the human reproduction process has to happen correctly. The steps in this process are:
- One of the two ovaries releases a mature egg.
- The egg is picked up by the fallopian tube.
- Sperm swim up the cervix, through the uterus and into the fallopian tube to reach the egg for fertilisation.
- The fertilised egg travels down the fallopian tube to the uterus.
- The fertilised egg attaches (implants) to the inside of the uterus and grows.
Factors affecting Female Fertility
Age

Age is the most important factor affecting fertility in women. As children, women are born with all the eggs they will ever have in their lifetime and the number of eggs available decreases each day from birth onwards.
While the decline is fairly gradual in young women, it gets much steeper as they grow older. Aside from a decrease in the number of eggs available, the quality of the eggs also declines as women age. This reduction in both the quantity and quality of available eggs means that older women are less likely to get pregnant and, if they do get pregnant, they are more likely to have a miscarriage.
Timing and Frequency of Sexual Intercourse

Most women have a 28-day menstrual cycle: this means there are 28 days between the start of one period and the start of the next period. Ovulation (when an egg is released from the ovary) occurs on day 14 of a 28-day cycle.
The fertilisation of the egg by a sperm depends on the day in the cycle in which intercourse occurs. The chance of getting pregnant is low at the beginning of the cycle and starts to increase from about day 8 onwards. Women are most likely to get pregnant if they have sex 2 days before they ovulate.
Once ovulation has occurred, the chance of getting pregnant decreases dramatically since sperm need to be present in the female genital tract prior to ovulation to increase the chances of getting pregnant.
Duration of Subfertility
![]()
The longer couples have been trying to get pregnant, the less likely they are to be successful. For example, a couple that has been trying to get pregnant for less than 3 years is almost twice as likely to get pregnant than couples who have been trying for more than 3 years.
Weight
Overweight women who have irregular periods are less likely to release an egg each month (ovulate) than women with regular periods. This means the chances of getting pregnant are reduced. Being overweight is also associated with an increased risk of miscarriage and of problems during pregnancy and delivery.
Smoking

Women who smoke are more likely to experience a delay in getting pregnant than non-smokers. Even passive smoking can be harmful. Smoking reduces a woman’s ovarian reserve (so her ovaries will have fewer eggs in them than a woman of the same age who does not smoke) and damages the cilia inside the fallopian tube, which are important for transporting the egg and/or embryo along the fallopian tube into the uterus.
Medical Conditions
Some women may have medical conditions that can affect their fertility. These conditions may be more general, for example thyroid disease and vitamin D deficiency whilst others may be more specific, for example, polycystic ovary syndrome (PCOS) and endometriosis.
Sexual History
Sexually transmitted infections such as chlamydia and gonorrhea can damage the fallopian tubes. Having unprotected sex with multiple partners increases your risk of a sexually transmitted infection that may cause fertility problems later.
Diagnosis
If you’ve been unable to conceive within a reasonable period of time, seek help from your doctor for evaluation and treatment of infertility. Both you and your partner should be evaluated. Your doctor will take a detailed medical history and conduct a physical exam.
Fertility tests might include:
- Ovulation testing. An at-home, over-the-counter ovulation prediction kit detects the surge in luteinizing hormone (LH) that occurs before ovulation. A blood test for progesterone — a hormone produced after ovulation — can also document that you’re ovulating. Other hormone levels, such as prolactin, also might be checked.
- Hysterosalpingography. During hysterosalpingography, X-ray contrast is injected into your uterus and an X-ray is taken to check for problems inside the uterus. The test also shows whether the fluid passes out of the uterus and spills out of your fallopian tubes.
- Ovarian reserve testing. This testing helps determine the quality and quantity of eggs available for ovulation. Women at risk of a depleted egg supply — including women older than 35 — might have this series of blood and imaging tests.
- Other hormone testing. Other hormone tests check levels of ovulatory hormones as well as thyroid and pituitary hormones that control reproductive processes.
- Imaging tests. A pelvic ultrasound looks for uterine or fallopian tube disease. Sometimes a sonohysterogram, also called a saline infusion sonogram, or a hysteroscopy is used to see details inside the uterus that can’t be seen on a regular ultrasound.